By Melanie Marshall
Leading voices in palliative care recently gathered in San Diego for the CSU Shiley Institute for Palliative Care’s National Symposium for Academic Palliative Care Education and Research, sharing the latest advances and strategies aimed at supporting patients and families experiencing serious illness.
The two-day event — “Quality in Palliative Care: Fusing Education, Research and Practice” — drew more than 220 faculty, clinicians, and researchers from across the country dedicated to enhancing palliative care, building the evidence base, and making palliative care accessible to everyone, everywhere.
Dan Johnson, MD, FAAHPM, National Physician Lead for Palliative Care at Kaiser Permanente’s Care Management Institute, delivered the opening keynote, saying “Palliative care is about connecting patients and families with providers who deeply care about them.”
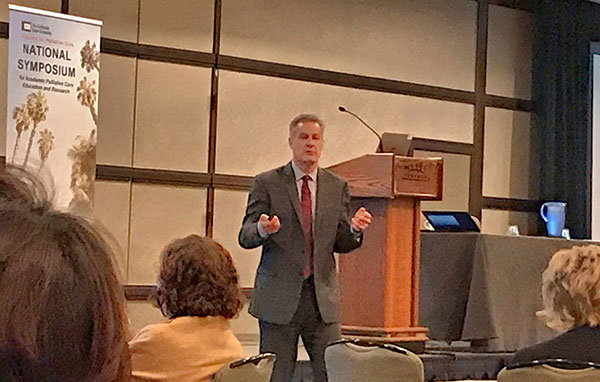
Dr. Johnson reminded attendees that educating others about palliative care is a shared passion and responsibility, and that high-quality teaching means removing barriers that can inhibit learning. For example, engaging learners around difficult topics like advance care planning works best when educators create a sense of urgency, minimize risk, and establish a safe space for discussion and practice, he said.
Recognizing Culture and Adapting Practice
Quality in palliative care also means addressing healthcare disparities and developing cultural competency so that all people can benefit from palliative care, several speakers said.
Respecting culture and diversity means learning to listen, being willing to make mistakes, and being open to new ideas, said Karen Bullock, PhD, LCSW, Professor and Head of the Department of Social Work at North Carolina State University.

“In some cultures, individuals receiving care don’t want to be the decision maker,” Dr. Bullock said. “Policies that don’t take into account culture can leave patients and families feeling like there’s no place for them.”
Dr. Bullock also emphasized that to achieve patient-centered care, providers must be continually learning and shaping their practice around each person and family they serve.
“If palliative care is truly tailored to each individual patient it means we must constantly be updating our knowledge and adapting our approach. We can’t learn one set of standards and apply them across the board,” Dr. Bullock said.
Addressing Healthcare Disparities
Tackling healthcare disparities also requires meeting patients where they are, said Marie Bakitas, DNSc, CRNP, NP-C, the Marie L. O’Koren Endowed Chair at The University of Alabama at Birmingham School of Nursing.
“In rural areas, palliative care isn’t located where the people are located,” Dr. Bakitas said. “Fourteen counties in Alabama have no hospice services.”
She said, “The road to palliative care for everyone, everywhere means addressing gaps in community-based, non-cancer, non-hospice palliative care, and weaving the threads of culture and diversity into practice.”
Collaborating to Grow the Evidence Base
Drs. Johnson, Bullock and Bakitas were among more than 110 educators, researchers and practitioners who shared their work at the Symposium through workshops and paper, poster, and plenary sessions.

Plenary speaker Dr. Jeri Miller, PhD, MS, MSc, the Chief of the Office of End-of-Life and Palliative Care Research (OEPCR) at the National Institute of Nursing Research (NINR) at the National Institutes of Health (NIH), inspired the crowd with an exhortation about the power of collaboration in expanding the evidence base.
Dr. Miller said quality palliative care research must exist in a context that is “highly public, deeply personal, and always dynamic in the way it influences policy.” She urged attendees pursuing such research to connect with NINR staff to talk about their projects and brainstorm ideas.
Funding New Research
Stimulating new research remains an important hallmark of the annual Symposium. The Gary and Mary West Foundation, in collaboration with the Institute, awarded nearly $50,000 in 2018 Seed Grants to five proposals designed to expand or improve the delivery of palliative care, particularly among seniors.
The projects ranged from one aimed at addressing the needs of caregivers of cognitively impaired older adults, to one examining the impact of palliative care referrals for discharged ICU patients, to another that would develop humanities-based curriculum to address death anxiety in medical students.

Seed grant recipients were Nidhi Mahendra, PhD, CCC-SLP, Associate Professor, Communicative Disorders & Sciences, Spartan Aphasia Research Clinic, San Jose State University; Kim Martz, PhD, RN, School of Nursing, Boise State University; Cara L. Wallace, PhD, LMSW, School of Social Work, St. Louis University; Kristyn Pellecchia, PMHNP, Assistant Professor of Family Medicine, School of Medicine, University of California Riverside; and Hyunjin Noh, MSW, PhD, School of Social Work, the University of Alabama.
Jennifer Moore Ballentine, Executive Director of the CSU Shiley Institute for Palliative Care, said the powerful work highlighted at the Symposium reflects exciting advances in palliative care, and the growing importance of the annual conference.
“The Institute is honored to provide a platform for innovative palliative care research and teaching that profoundly impacts the lives of seriously ill patients, families, and the providers who care for them” Ballentine said. “The collaboration inspired at this remarkable Symposium is truly elevating our field.”
Supporting Family Caregivers
The drive to increase quality palliative care is fueled by a deep desire to ease suffering of vulnerable patients and families, several speakers noted.
A plenary panel facilitated by West Health Chief Medical Officer Zia Agha, MD, focused on how to support family caregivers of seriously ill seniors. The panel included Jennifer Wolff, PhD, Professor of Health Policy and Management at the Johns Hopkins Bloomberg School of Public Health, John Hopkins University; Kathleen Kelly, MPA, Executive Director, Family Caregiver Alliance, National Center on Caregiving; and Theresa Harvath, PhD, RN, FAAN, Executive Associate Dean at The Betty Irene Moore School of Nursing at UC Davis.

The panelists highlighted the tremendous impact of family caregivers on today’s healthcare system and the significant challenges such caregivers often encounter. Many family caregivers are providing complex care with no medical training and little support or reinforcement, the experts said.
“It’s important for healthcare providers to tell family caregivers that self-care is a requirement of the job,” Dr. Harvath said. “It can’t be optional if they’re going to be in it for the long haul and want to come out on the other side.”
Symposium Continues to Grow
The record number of attendees at the 2018 Symposium represented more than 75 universities and healthcare organizations, reflecting the growing impact of the event and the Institute that created it.
First launched in 2013 as a CSU-only event that drew roughly 30 participants, the Symposium has since transformed into a national conference drawing palliative care educators and practitioners from as far away as South Africa.

The 2019 National Symposium for Academic Palliative Care Education and Research will be held Oct. 11-12 at the Sheraton Harbor Place Hotel in San Diego. For more information, see https://csupalliativecare.org/symposium.




