Interprofessional Education Helps Build Strong Palliative Care Teams
When Brian (last name withheld for privacy) was treated for cancer at the Mayo Clinic in September 2019, his palliative care team worked together to provide him not only relief from his physical pain but also emotional comfort.
That team approach – a hallmark of palliative care – not only provided an extra layer of support to Brian, but to his wife Lynn. “They really advocated on our behalf within the complex system of Brian’s treatment,” she said.
Brian’s care team was part of an interdisciplinary team (IDT) model that typically includes a physician, a nurse, a social worker, and other healthcare professionals. His story is highlighted in a Sept. 10, 2019, Mayo Clinic Educational YouTube video, “Palliative Care for You and Your Family.”
Working as a Team
“The crux of palliative care is a team-based approach to care, really aimed at treating the physical symptoms as well as the emotional and spiritual symptoms of a serious illness,” Jacob J. Strand, MD, a palliative care physician at the Mayo Clinic, says in the video.
An IDT alliance such as the one employed at the Mayo Clinic relies on health professionals from different disciplines, along with the patient, working collaboratively as a team. The most effective teams share responsibilities and promote role interdependence while respecting individual members’ experience and autonomy.
Healthcare professionals who are part of an IDT need specialized training on how to communicate with each other. They also need to understand both the verbal and non-verbal clues that patients and their families show during times of serious illness, according to Shirley Otis-Green, MSW, MA, ACSW, LCSW, OSW-C, FNAP, a licensed clinical social worker and founder of Collaborative Caring.
“Palliative care specialists will never see all of the patients with advanced illness,” Otis-Green said in a 2019 blog post for the CSU Shiley Institute for Palliative Care. “That’s why educating all staff in generalist palliative care skills is so important. Once you’ve been trained to ask the right questions and listen for the clues, your awareness changes.”
Nurses Play a Crucial Role
All disciplines involved in the care of a patient collaborate to develop the patient’s plan of care, and each team member provides critical input. The patient and family are included in the development, implementation, maintenance, planning and evaluation of the care provided.
While physicians typically lead an IDT, nurses also play a crucial role by solve patient care problems and to provide the optimal quality level of care to the patient or group of patients.
In addition to their clinical abilities, nurses who are effective team participates must excellent interpersonal and communication skills, respect for others, the ability to establish and maintain trust, critical-thinking skills, problem-solving skills, decision- making skills, and the ability to understand and identify the contributions of others that can improve the quality of the patient’s care.
Chaplains Contribute to an IDT
Patients with serious illness often benefit from spiritual/emotional care regardless of their faith or belief system. Chaplains, rabbis, or other spiritual care providers are a valuable part of an IDT.
Still, “many chaplains are quietly apprehensive about actually joining an interdisciplinary team,” writes Gordon Hilsman, BCC, on the National Association of Catholic Chaplains website.
“…What often keeps chaplains on the periphery is lack of confidence — confidence in oneself, one’s pastoral identity, and one’s ability to stand with other team members as valued professionals able to make regular contributions to the primary work of that team and hospital unit,” Hilsman writes.
To combat this apprehension about teamwork, he recommends that chaplains learn how to concisely record patients’ stories and describe in easy-to-understand language how patients feel about their spiritual lives.
Social Workers Keep it all Together
Patients who need palliative and/or hospice care can feel depressed, angry and anxious besides suffering from profound physical pain. In addition, they can be worried about money, feel socially isolated and get into disagreements with their family members.
Because of these challenges, palliative care social workers can effectively guide patients and families in navigating the many challenges and pitfalls of severe illness. They can also point out ways to help them with the difficult process of end-of-life planning.
“Palliative care is a supportive service that acknowledges and supports the whole person, the human being experiencing serious illness,” said Elizabeth Robinson, MSW, a palliative care social worker in San Diego. “I think that’s the most important takeaway. Who are you beyond this diagnosis? Let’s start there.”
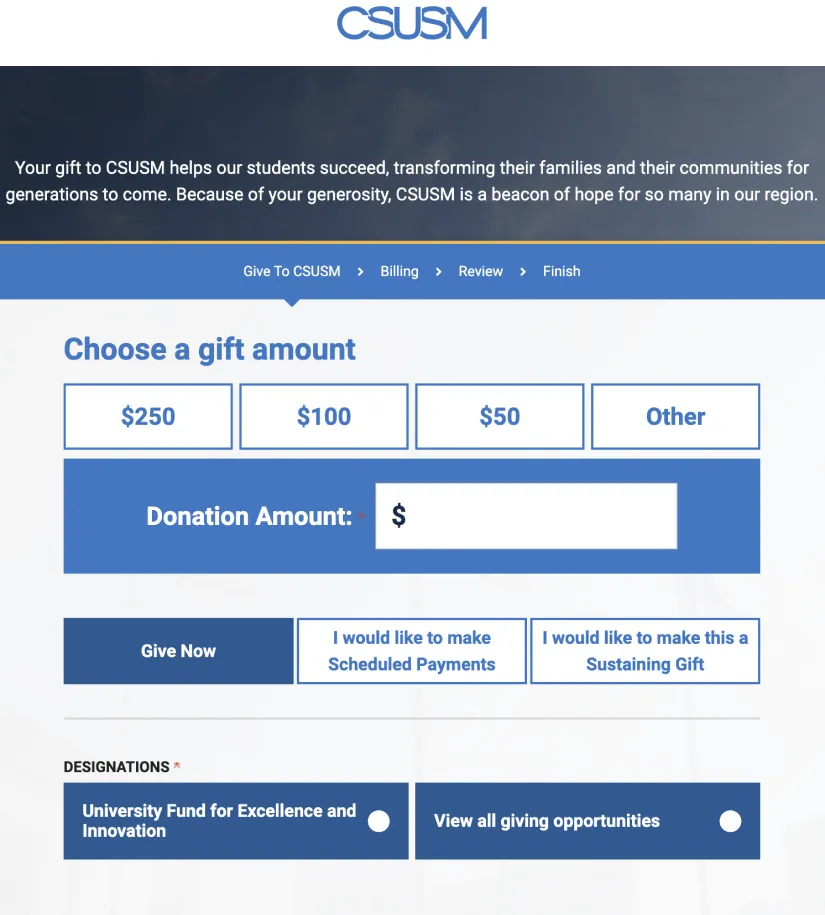
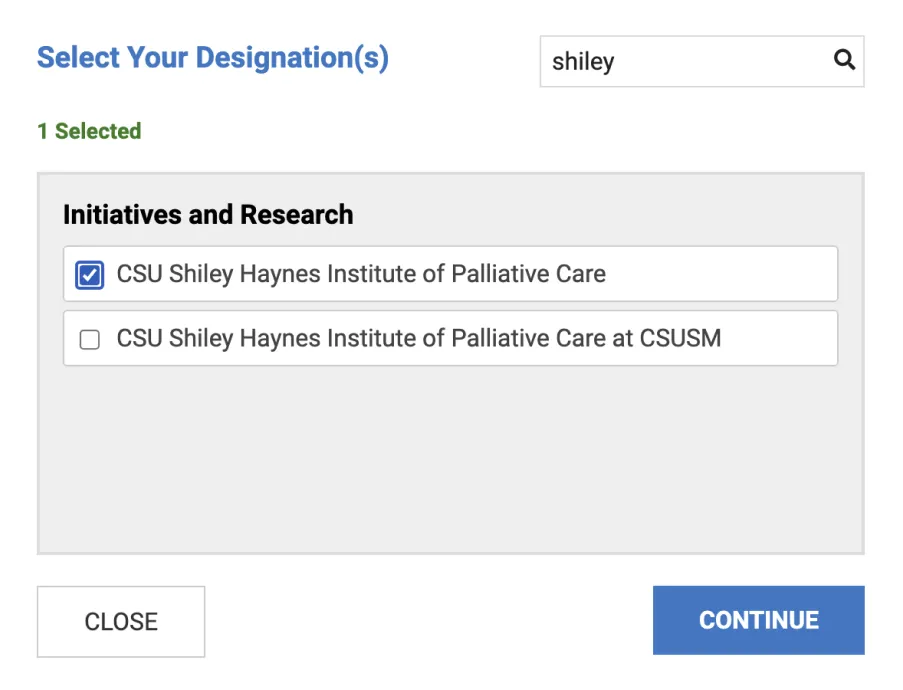
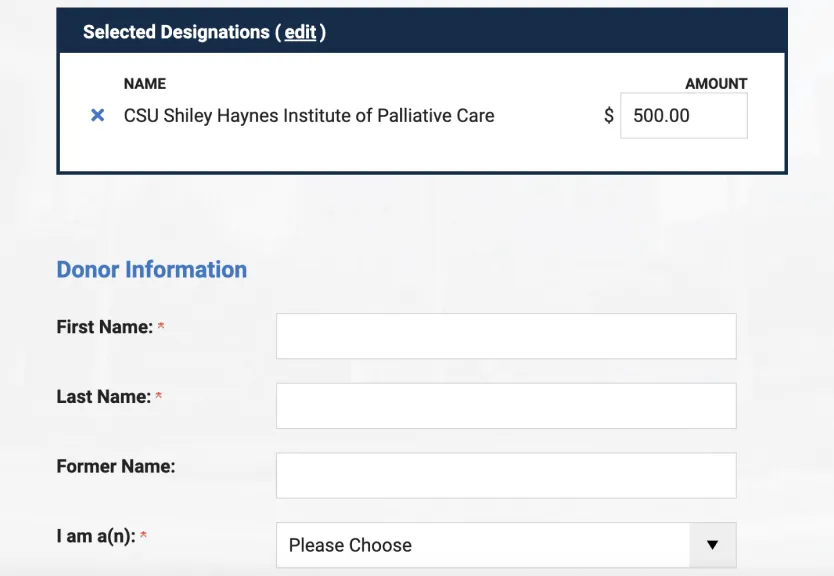
Interprofessional training can be extremely valuable in strengthening palliative care teams. The CSU Shiley Institute for Palliative Care offers a self-paced, online Core Concepts in Palliative Care curriculum designed for that purpose, as well as a variety of instructor-led online programs.