Guest Contributor: Kathy Brandt
Most of us working in palliative care and hospice have a passion for the work we do. We believe that the healthcare system places a higher value on efficiencies and cost savings than it does on providing holistic care or improving quality of life for patients and families. Don’t get me wrong, we all know highly compassionate and skilled professionals working in every aspect of healthcare, it is the system itself that is fractured.
Palliative care flips the model – palliative care:
- Emphasizes the identification of patient goals
- Invests time in determining the medical, social, spiritual, economic, and environmental barriers to achieving those goals and
- Deploys a team of professionals to work with the patient and family to develop and implement a care plan to mitigate those barriers
Luckily for us, the healthcare system is evolving, with the overarching goal to achieve the Triple Aim: Improving the patient experience of care, improving the health of populations; and reducing the per capita cost of health care. As a result CMS, and by default healthcare systems, providers, and payers, is motivated to invest in new models that can achieve the Triple Aim goals.
In order to “make the case” for community-based palliative care we must be able to demonstrate the efficacy of the care provided, refine our model as it evolves, develop a strong financial case, and improve the care provided to each and every patient and family served. None of that can happen without data. In other words, we need metrics.

Will Your Palliative Care Program Save Money? Does it Improve Care Outcomes?
Selecting the right measures to use for your program can be daunting. In the online course, Metrics and Measurement for Palliative Care, J Brian Cassel and Kathleen Kerr have identified five steps for selecting palliative care metrics:
- Review best practices in the palliative care field
- Elicit and understand stakeholder priorities
- Identify potential structure, process and outcome metrics
- Assess feasibility – consider data collection burden and data accessibility
- Pick your portfolio of feasible measures
1. Review best practices in the palliative care field
Best practices can be found in the National Consensus Project for Quality Palliative Care Clinical Practice Guidelines for Quality Palliative Care, which identifies eight domains and best practices. If you are in the nascent stages of building your palliative care program, review the NCP Guidelines and integrate those best practices into your systems, processes, and staff education.
2. Elicit and understand stakeholder priorities
Your community-based palliative care has many stakeholders – including the patients and families you serve, the other healthcare and human services providers who refer patients and are involved in the plan of care, health systems, and payers. Each of these stakeholders has different expectations of your service. In order to achieve the Triple Aim you must determine what’s important to the stakeholders who are receiving the care, providing the care, and paying for the care. You do that by asking them what’s most important to them.
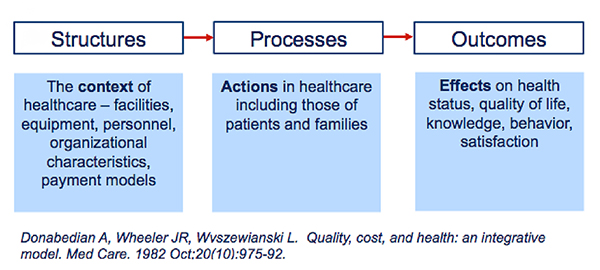
3. Identify potential structure, process and outcome metrics
Of all of the steps, this one can seem the most daunting. How do you know what to measure? Brian and Kathleen’s course describes the importance of the Donabedian model of measurement and potential metrics to address each of these measurement domains.
Examples of palliative care measures include:
Program Staffing
- Process
- Volume and characteristics of those approached or seen
- Outcome
- Control pain and other physical symptoms
Services offered
- Process
- Timing of first contact relative to diagnosis and/or death
- Outcome
- Decrease family members’ depression, anxiety, distress
Locations/ settings/availability
- Process
- Proportion patients receiving a comprehensive assessment
- Outcome
- Number of ED visits last 30 days of life
| Structure | Process | Outcomes |
| Program staffing | Volume and characteristics of those approached or seen | Control pain and other physical symptoms |
| Services offered | Timing of first contact relative to diagnosis and/or death | Decrease family members’ depression, anxiety, distress |
| Locations/ settings/availability | Proportion patients receiving a comprehensive assessment | Number of ED visits last 30 days of life |
There are numerous sources where you can find validated measures for community-based palliative care including:
However the best place to look is the California Health Care Foundation’s Palliative Care Measure Menu. The tool allows you to quickly and easily quality measures based on the unique characteristics of your program, care setting(s), and partners.
4. Assess feasibility – consider data collection burden and data accessibility
This point can be summarized as: if you can’t collect it or won’t use it, don’t measure it. At first glance it may seem like a great idea to select a large number of measures so that you can be certain to measure the “right things.” That is a common mistake! Instead, start with a small number of measures. And as you select each one, be sure to ask
- Who needs this data and how will they use it? Will it be used to:
- Prove the case for palliative care?
- Improve the care delivered to patients?
- Refine your processes to improve care or efficiencies?
- How hard will it be to collect this data?
- Who owns the data – a partner or us?
- Do we already capture the data in our documentation?
- Can we easily report out and analyze the data?
5. Pick your portfolio of feasible measures
According to Brian and Kathleen, “Minimal measuring includes 12-14 items addressing quality, plus operational metrics,” based on the needs of your stakeholders.ConclusionSelecting the exact right measures for your program isn’t easy because the metrics you pick must be the right ones for your program and your stakeholder partners. The good news is there are a number of resources to help you, including those already referenced as well as a comprehensive online course developed for the Institute by Brian and Kathleen, Metrics and Measurement for Palliative Care. In addition, Brian and Kathleen also developed Creating Data-driven Proposals and Presentations for Your Palliative Care Program, and The Business Case for Palliative Care. Each of these courses contains in-depth, practical information to help you grow and improve your program.




