Community Health Workers Offer Access to Underserved Groups
Before COVID hit, Resolution Care Network – a telemedicine palliative care service in Eureka, Calif. – employed community health workers (CHWs) as an extension of its interdisciplinary palliative care team. “They were the agency’s feet on the ground, its eyes and ears in the field,” said CEO Michael Fratkin, MD.

Though COVID safety measures required a reformulation of their roles, CHWs “remain highly effective coordinators of care,” Fratkin said. “Post-pandemic, we’ll put them back into the field.”
Sometimes called care navigators, lay health workers, or promotores de salud, CHWs are getting increased attention as frontline health educators.
In palliative care, their paraprofessional role could help answer a pressing question about how to better reach underserved communities, particularly in a time of increased attention to healthcare access and equity.
Fratkin said CHWs can be an invaluable resource. “These are individuals who are super-talented caregivers,” he said. “When we look at the emerging elder tsunami, and people in our field burning out, this is an opportunity to reach into the community and identify those who can be trained for this role.”
Studying the Impact of CHWs
CHWs are defined by their practical skills and talent for problem-solving, not by professional degrees or formal credentials. Palliative care agencies are challenged to identify, recruit, orient, train, deploy, and supervise those who could have a big impact on their service delivery.
“It requires an organizational culture that allows the right people to arise from the community,” Fratkin said.
One of Resolution Care Network’s CHWs became skilled in dealing with grief issues, Fratkin said. Another had previously been a birth doula and had an interest in this field. A third reached out to notify the palliative care social worker when a patient was ready to accept a referral to alcohol detox.
Fabian Johnston, MD, a surgical oncologist at Johns Hopkins School of Medicine in Baltimore, Md., is the principal investigator of a grant from the federal Agency for Healthcare Research and Quality to study the impact of “culturally informed patient navigation.” Johnston’s study focuses on CHWs (navigators) promoting earlier utilization of palliative care in African American communities, which have worse healthcare experiences and outcomes across a spectrum of settings and diseases.
His research – including in-depth interviews and stakeholder focus groups – concluded that CHWs can help to improve disparities, achieve quality outcomes for traditionally underserved patients, and address the domains of palliative care with patients and families in a culturally sensitive manner.
What’s important, Johnston said, is to normalize this kind of care further upstream, introducing concepts of advance care planning, advance directives and POLST and explaining palliative care and hospice. “We’re still studying it, but we have seen multiple groups implement and utilize the CHW in improving palliative care.”
There is additional research demonstrating the impact and reach of CHWs:
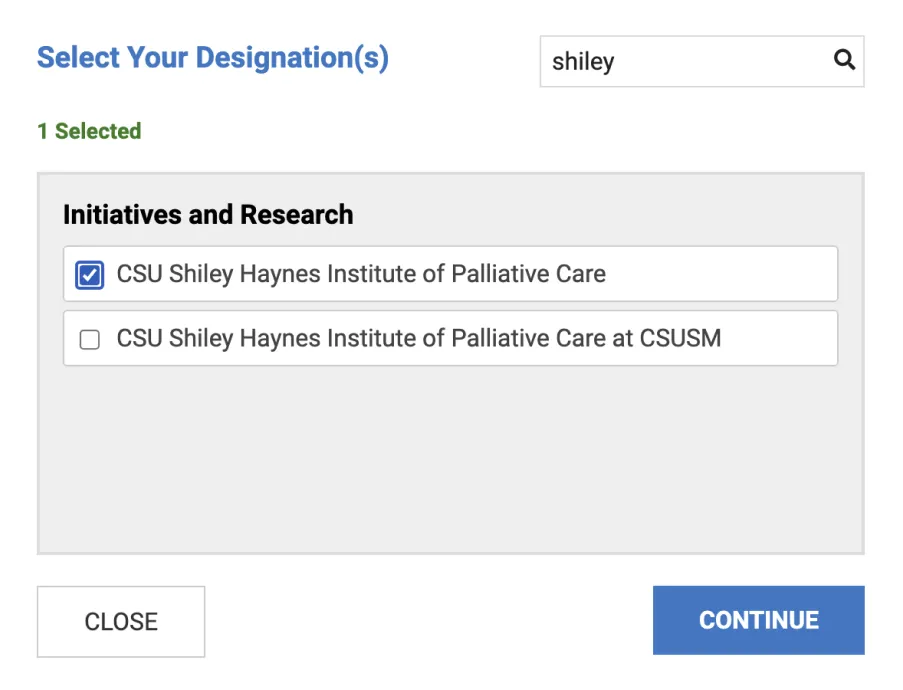
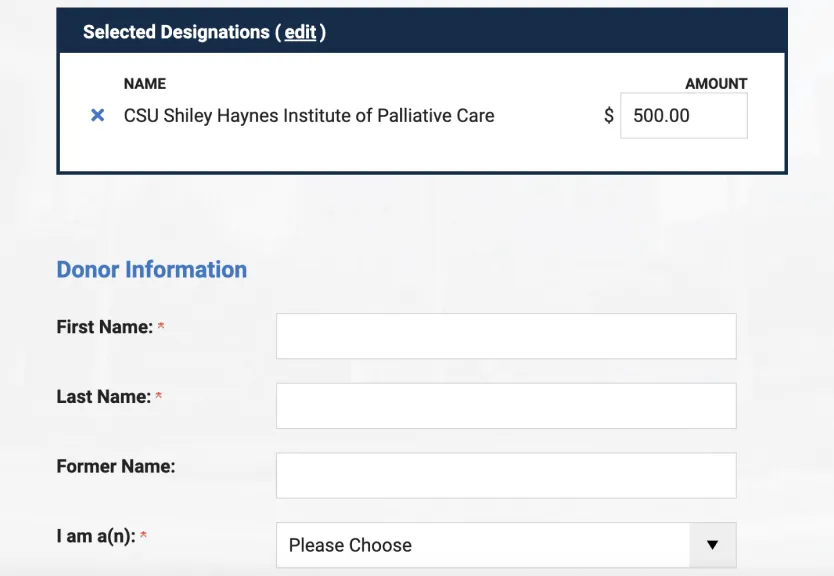
- At California State University Long Beach, nursing professor Joy Goebel, RN, PhD, FPCN, led a study published last year in the Journal of Palliative Medicine on improving palliative care awareness in the Latino community through promotores de salud (CHWs). The study was funded in part by a grant from UniHealth Foundation through the CSU Shiley Institute for Palliative Care. The study showed promotores were effective at providing families with important information about palliative care related to chronic disease management.
- Richard Crespo of the Marshall University School of Medicine in Huntington, W.Va., studied the provision of ongoing behavioral support using CHWs for high-risk diabetes patients in rural Appalachia. The study showed CHWs can be a valuable component of healthcare services.
- Gabrielle Rocque at the University of Alabama-Birmingham (UAB) found that navigators significantly reduced costs, emergency room visits, and hospitalizations—all of which can make even greater contributions as the health system transitions to value-based care.
Historically Underserved Communities
J. Nicholas Dionne-Odom, PhD, RN, a nurse researcher at UAB, has studied how to increase access to care in historically underserved communities in the Deep South.
“In my clinical trials, we use lay navigator coaches with family caregivers of patients who have advanced cancer,” he said. “This is a culturally appropriate way to gain access by tapping into a lay workforce from the community.” It can also extend the reach of palliative care organizations that don’t have sufficient professional staff.
Some in palliative care might be concerned about scope-of-practice issues, Dionne-Odom said. These can be addressed by integrating CHWs as part of the interdisciplinary palliative care team, giving them adequate supervision, and developing protocols to define the boundaries of their practice.
“The kind of care they deliver can be equally beneficial to a lot of folks—and they can triage those who have greater needs to the right specialists, who are no longer tied up doing things that could have been addressed by lay health workers,” he said.
“The best CHWs have large social networks. They know a lot of people. They are community influencers,” he said. “They have a deep understanding of cultural issues surrounding health and how to build trust with communities.”
But any lay-inclusive care model needs a robust clinical supervisory component, he said. “From us, they receive weekly structured oversight. They communicate with and alert the interdisciplinary team if certain issues arise, such as questions involving medications or worsening symptoms.”
CHWs or navigators can be cost-effective to the overall service, but they aren’t typically covered by traditional reimbursement. That’s where health plans can give leeway to frontline providers to utilize the services that make the most sense for each patient or situation, Fratkin said.
“They tend to stay quiet unless you create a team culture that invites their participation,” he added. “Otherwise, they know they don’t have that much status. To maximize their value takes a lot of invitation. Our job is to support them and offer a bit of guidance.”
Some people have an amazing talent for this work, he said. Is that emotional intelligence? “I think it’s more than that. People with these gifts have been taking care of the dying in their communities since time immemorial.”
How did Resolution Care Network recognize good candidates? “We built our program from the bedside up. We were attuned to what was happening on the ground. We knew where things were working well on our cases and who were the amazing family caregivers or paid caregivers.”