May was hardly a slow news month—volcanic eruptions in Hawaii, North Korean diplomatic back-and-forths, the royal wedding, another tragic school shooting—so you can be forgiven for not noticing that California’s End of Life Option Act was overturned. The Riverside County Superior Court decision was immediately appealed, but a stay was not granted.
For now, while the appeals process plays out, the law offering a legal process for physicians to prescribe a lethal dose of medications for terminally ill, competent patients has been ruled unconstitutional and void. Needless to say, this has created a new turmoil in the palliative and end-of-life care environment here in our home state. While the specifics are local, the issues are national.
Palliative Care Eases Suffering
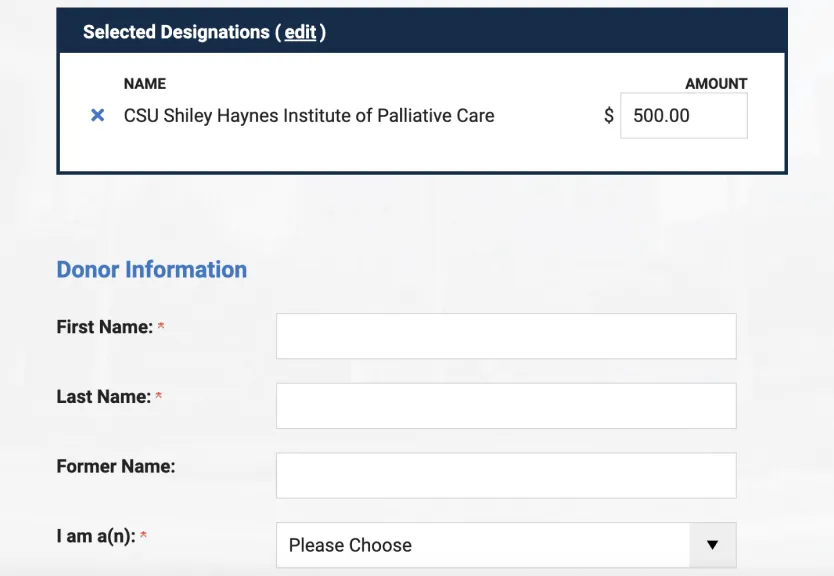
The CSU Shiley Institute for Palliative Care has no position on End of Life Option Act (EOLOA) or the place of medical aid in dying in the landscape of palliative care. But we are acutely aware of how the conversation surrounding it continues to highlight the ongoing challenges patients with serious and terminal illness and their families face in finding support and relief from suffering of all kinds, not just in California, but across the country.
As a recent conference in Sacramento sharply highlighted, we’ve made progress toward meeting the needs of our state’s seriously ill residents and their families, but we still have a long way to go. So far, estimates suggest that about 500 to 700 patients may have utilized medical aid in dying since the California EOLOA took effect in June 2016. That’s less than 0.15 percent (0.00145) of the total deaths in the same two years.
Meanwhile, 77 percent of the roughly 481,260 Californians who died in the past two years succumbed to heart disease, cancer, stroke, Alzheimer’s disease, lower respiratory disease, diabetes, liver disease, or hypertension. These are exactly the conditions for which palliative care can be profoundly effective in improving quality of life, relieving pain and distress, supporting families, and affirming patients’ preferences.
The Challenge of Accessibility
And yet, in most areas of the state, there are fewer than 35 hospice and palliative medicine board-certified physicians for every 100,000 population. Up to 80 percent of our hospitals offer some form of palliative care, but the team size and composition, services and accessibility vary greatly. Our roughly 600 hospices care for close to 45 percent of all Medicare beneficiaries prior to death, but half for less than a month.
Patients who need us don’t know about us, don’t know how to ask for us, and don’t know what they are getting when they do find us. The systems and structures that support us, don’t do so nearly well enough. This has to change—not just for the few hundred people now unable to access medical aid in dying, but for the hundreds of thousands who never would and badly need our care.
Time to Expand Palliative Care is Now
In the midst of the turmoil over the status of the EOLOA, we must all redouble our efforts to expand awareness of palliative care. I challenge our hospice and palliative care providers to take the opportunity to trumpet the benefits of their services, their aggressive treatment of pain and suffering, their commitment to patient-centered, whole-person care for patients and families.
I also challenge the health systems, payers, providers, and policymakers to quadruple efforts to ensure that every resident of our state has access to comprehensive palliative care from the hands of properly trained, skilled, and compassionate clinicians. Now is the time—Again! Still! Perhaps by the time the appeals process plays out for the End of Life Option Act, the option will no longer be needed.