Teaching Primary Palliative Care in a Large Health System
In large sections of this country there is virtually no access to specialized palliative care for many seriously ill patients, said Jeffrey Greenwald, MD, a hospitalist and medical educator at Massachusetts General Hospital, Boston (MGH). The Boston area, and particularly the Mass General Brigham system, are relatively resource-rich with palliative care expertise. But getting basic palliative care training to clinicians on the floors and in the clinics has required a determined effort supported from the top.
Dr. Greenwald is Associate Director for Implementation for the Palliative Care Continuum Project at MGH, a culture-change initiative supporting interprofessional clinicians who care for patients with serious illnesses and their families with specialized training to enhance their communication skills. It uses the Serious Illness Care Program, a system-level model developed by the palliative care experts at Ariadne Lab, to roll out training on how to lead goals and values conversations with seriously ill patients in a variety of inpatient and outpatient settings across the system.
There are logistical and cultural challenges to teaching palliative care across a system, Dr. Greenwald said. “As in everything, culture eats process for breakfast. You can’t just walk in and expect them to start changing behavior.” Logistically, reimbursement for having goals-of-care conversations with patients is improving implementation, but slowly. There are documentation requirements and electronic health record issues, but these are not insurmountable. “There is also a fear of opening a can of worms to a bunch of other issues.”
The difficulties in disseminating palliative care learning are not because professionals don’t think it’s important, he added. “Culturally, it’s common to point to someone else who should be responsible for it, instead. The oncologist should do it, or the primary care physician, or the hospitalist. People say, ‘I know how to do it, but I don’t have the time. And I don’t know what to do if the patient starts crying’.”
It should be within any health professional’s wheelhouse to address basic symptom management and care preferences. But for residents and inexperienced clinicians, a goals-of-care conversation too often is agenda-driven, merely trying to get code status, dialysis or not, CPR or not—without a deep dive into the patient’s values and priorities. “With training we can be a little more nuanced,” Dr. Greenwald said.
“Our messaging to clinicians is: ‘We’re not here to tell you you’ve been doing it wrong. We’re here to give you a structure and tips and tools to help you when things get difficult. This is something you can integrate into your current practice’.”
The Primary Track
Palliative care experts have been saying for years that the demand and need exceeds the availability of trained palliative care specialists. Instead, basic skills in primary palliative care—principally leading conversations about the patient’s values and goals for treatment and providing serious illness symptom management—need to be taught to bedside clinicians. They could then routinely address their seriously ill patients’ immediate palliative needs while reserving the more challenging and complex cases for specialized palliative care teams.
Other examples of organized approaches to teaching primary palliative care include Vital Talk, which offers a train-the-trainer approach to disseminating skills in having difficult conversations, delivering serious news, and communicating effectively with seriously ill patients.
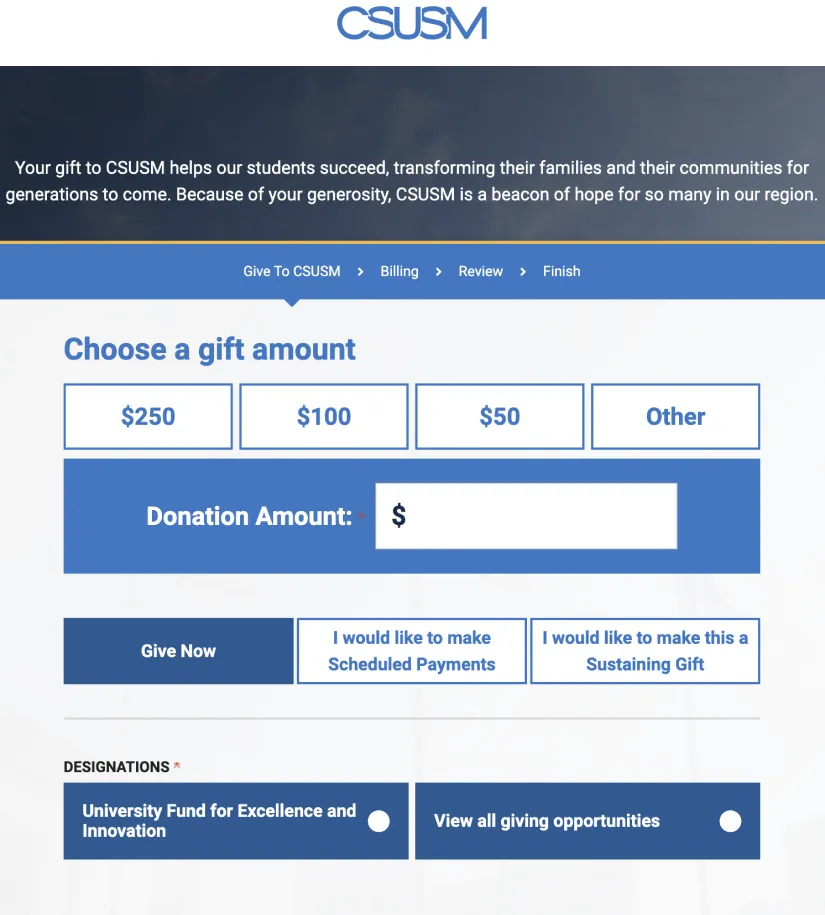
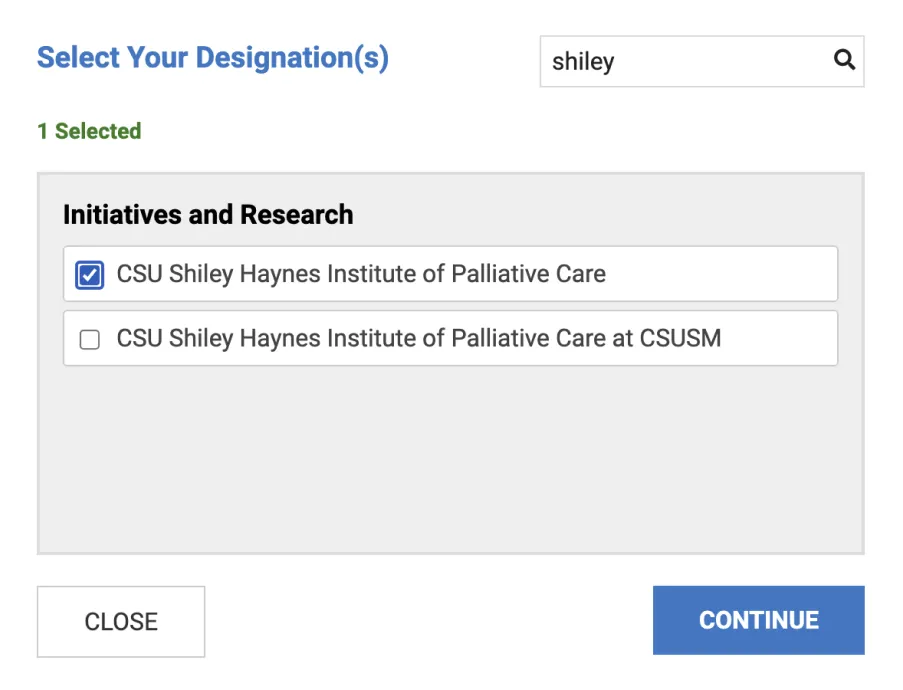
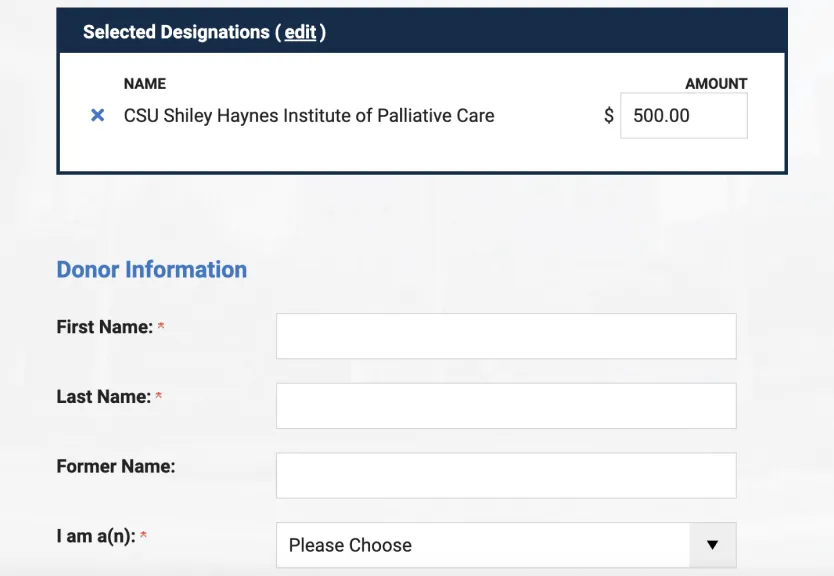
The California State University Shiley Haynes Institute for Palliative Care offers a comprehensive, self-paced, online curriculum in primary palliative care for all providers. Its series of interactive online courses for clinicians in any practice setting covers concepts of palliative care including clinical approaches to pain and symptom management, strategies for improving communication, empowering patients in healthcare decision-making and integrating these into current primary care practice—in 24.5 hours of self-paced coursework. But getting people on board is difficult for all the usual reasons, explained the Institute’s executive director, Jennifer Moore Ballentine, MA.
“We would agree that it is absolutely essential for every clinician to have a basic toolkit of palliative care skills and a whole-person approach to anyone with serious illness,” Ballentine said. “Many primary care clinicians are already ‘doing’ palliative care but need to hone specific skills in communication around discerning the patient’s goals for medical care, assessing psycho-social-spiritual distress, and being aware of when to refer to specialists. This means looking not just at the disease but at the patient as a person in the context of their individual goals and their loved ones, their culture and social location,” she said. “That sounds simple… but it’s not easy.”
A Reasonably Productive Conversation
The Ariadne approach offers a scripted conversation about goals of care, Dr. Greenwald said. Palliative care “scholars” who have received additional training help to lead workshops within their medical specialty. “We say you can have a reasonably productive conversation in 12 to 15 minutes. And you can also enlist other members of the care team to help.”
The Continuum Project has been able to tailor training to different care groups and patient populations while teaching process improvements and data gathering,” he said. It trained more than 1,300 interprofessional clinicians from 2017 to 2019.
Michael Nathan, MD, an internist and primary care physician at MGH’s Revere HealthCare Center, was tapped as a Primary Care Palliative Care Champion by the Continuum Project and took the Primary Care Education Program. Since then, he has been a frequent facilitator for Continuum’s Serious Illness Conversation training groups. Dr. Nathan said he already had an interest in the topic, has done hospice medicine, and once considered pursuing a fellowship in hospice and palliative medicine.
“I’d like to think we’re doing pretty well in our system at addressing patients’ symptom management needs,” he said. Within general internal medicine, many clinicians are experienced at prescribing opiates for pain, for instance. “We manage a lot of chronic pain patients. Clinicians here also get it that opiates can be used in advanced pulmonary disease.” There is discussion going on in the system about having earlier conversations with patients about what matters most to them, how to structure meaningful conversations, and how to introduce advance directives, he said.
“At Mass General, we have trained all the PCPs and residents. Any clinician who has been in the system for at least four or five years has had the opportunity to practice the Serious Illness Care model in a simulation with an actor.”
Whatever the model or training approach selected, ensuring clinicians in any setting caring for patients with serious illness have communication and symptom management skills is a top priority that requires an internal champion and follow through.